A Guide for Physicians
and Other Healthcare Providers
Grief Reactions Associated with Prolonged vs. Short Illness: A Case Study and Analysis

Concerning the Time Elapsed between a Life-threatening incident and Death
by Richard Easton, MD
Setting: Memorial service for a deceased person,
A haughty visitor speaks very judgmentally
to the spouse of the deceased:
“Well, you’re in good spirits and sporty bright clothes,
laughing and mingling with the crowd
like this is one great cocktail party!”
How the Incident/DX-Time-to-Demise (I/DTimetoDemise) determines and complicates social interactions
I deal here with a neologistic term: a discussion of the Incident/DX-Time-to-Demise spectrum idea. [Defined as the time of initial diagnosis or awareness of a terminal condition to the actual death of the individual. - Ed] The discussion does not concern itself with the 'five stages of loss,' nor the sequence-vs-overlap of one Kubler-Ross[1] stage over the other nor the correctness of the K-R "five stages" theory nor whether there are really any stages at all.
This essay presents the characteristics of the time span itself, i.e., how much time has passed in the eyes of various people impacted by the death of a person.
The characteristics of that time span include:
- Compressibility, Duration and Expansion of Time;
- Forewarning;
- Contemporaneous Support during the demise;
- The Individual, Personal Reaction to death;
- The Time for Reflection and Resolution of Feelings; and,
- The Time when the Undeniable Reality of “It’s Over, The Deceased is Never Coming Back” overtakes all other concerns and becomes shatteringly real.
The Perceived Duration, Compressibility, and Expansion of Time
The measurable duration of time, i.e., the time during which survivors can assimilate the death of a victim after an incident or diagnosis may be short or long. The incident may be so powerful that it compressed time and causes instantaneous death (e.g., electrocution or a massive heart attack.) The Time-to-Death is compressed to minutes or milliseconds.
Alternatively, the duration between being given a fatal disease diagnosis and succumbing to death can expand subjectively to near-interminable proportions. This is a common result when the physical and mental deterioration takes place over months or years (e.g., as in progressive chronic obstructive pulmonary disease [medical name for COPD is almost as long as the disease course], or due to dementia**[name is short, but the agony is as long as COPD]).
The Short Duration of I/DTime-to-Demise can be due to extrinsic factors, e.g., an instantaneous event like a fatal gunshot or when a patient is “HbaB” (Hit by a bus) or other vehicle at high rate of speed. Or the event I/D Time-to-Demise may be due to an intrinsic etiology such as a fatal heart attack, major cardiac arrhythmia or stroke.
A Long I/DTime-to-Demise is precipitated by chronic disease situations. Chronic diseases (specifically incurable) may be treatable, but only to the extent they prolong life and patient agony (no less to the agony of the care-givers) and delay the inexorable, destructive decline of the condition. This long-term prolongation of the condition and its associated medical and emotional misery has the effect of transforming the ancient Chinese concept of Death by A Thousand Cuts [2] into a minute-by-minute real-time reality [3] for all concerned.
Death by a thousand cuts can be thought of as a specific, insidious type of failure, in this case the global failure of all our attempts to avert it, and ultimately, patient death. Generally speaking, the death that occurs is a result of many small problems, such as a series of drug trials that fail, one after another, each failure representing a “cut.” For the patient, the death occurs is a result of many small problems, such as a series of physical insults, one after another, as in vascular dementia or multi-infarct dementia. Each infarct, no one of which is fatal, reveals itself as a new “cut” (AKA damage) to one or another vital sections of the brain. Each cut deep in the brain reveals itself outwardly to medical and family observers as loss of function due to destruction of a specific area in the brain. That functional loss could be aphasia (expressive or receptive), agnosia, prosopagnosia, paralysis of a limb, visual malfunction (of visual pathways or visual cortex damage), onset of verbal word salad, mild-to-major loss of one or another segments of short-, medium- or long-term memory. Each “cut” leads to an observation, each observation drains a bit of another intellectual or physical ability, and the cumulative awareness of those losses leads to a growing emotional burden, ultimately causing a severe drain of emotional and physical energy on the participant-observers.
The End of Life processes in our culture, i.e., illegal status of euthanasia, and societal agreement (or at least acquiescence to the idea) that we should “let Nature takes its course” without our intervention, has solidified the prolongation of agony of both patients and care-givers by prohibiting use of means to address the Quality of Life issues surrounding EOL situations.
When proven, objectively documented and independently verified (two or more experts), predictions of inescapable death within a finite period of time, is employed as part of the decision-making process the outcome for all has been beneficial. The objective assessment of a terminal condition has provided the impetus for a most empathetic alternative, The Hospice Movement. In Hospice philosophy, Quality (Not Duration or Extension) of Life, is of paramount importance.
Hospice Care[4] is designed to give supportive care to people in the final phase of a terminal illness and focus on comfort and quality of life, rather than cure. The goal is to enable patients to be comfortable and free of pain, so that they live each day as fully as possible.
Importance of Awareness
Awareness of the following ideas is essential in understanding individual and group responses to death. Specifically:
- Forewarning of coming events is essential to preparation for coping with the future;
- Contemporaneous Personal Support during the events before, during and after demise are vital to implementing coping mechanisms to work and not be interfered with by emotional overflow or physical collapse;
- The Individual, Personal Reactions to death may not be predictable, but their variability and the unpredictability of the responses should be anticipated and taken into account during planning, formal or informal; and finally, consideration must be given to:
- The Time for Reflection and Resolution of Feelings by the members involved in the completion of the post-demise exercise, whether it be funeral, memorial service, cremation, no gathering or intimate service.
With these considerations as background to the discussion, we continue:
The I/DTimetoDemise (abbrev: “Time”) spectrum is of significance, whether they have contemplated it or not, to the by-standers, all healthcare workers, other care-givers, and all family and friends of the deceased. The significance of “Time” spectrum awareness is critical to the future emotional state of the survivors, irrespective of their personal, professional or tangential point of view of the situation.
The level of significance to the involved survivors is proportional to the “Time” that each person has experienced between learning of the death and interaction with other participants in the situation.
One focus is: The group with the longest-term relationship and early knowledge of the pending death would be (aside from the medical team making the diagnosis) the patient and family members. Their Time for Reflection and Resolution of Feelings would be the longest. They would have experienced the immediate rush of feelings when given the facts of the case. This information could be viewed as the earliest Forewarning of coming events, giving them the longest period of time for Reflection on themselves, the family and others, thoughts about the impact(s) of the disease and life-changes about to come to pass. Conflicts of all sorts, emotional, financial, major, minor would surface in the normal course of events. Reflection over time would be a real advantage when faced with Resolution of the various complications that arise. For those who are Forewarned, have the necessary Contemporaneous Support, have the standard range of Reactions and are free of unusual psychological interpersonal relationships, and have time to Reflect and Resolve any issues dragged up by the loss, the “left-sided curve” (Mode) below probably applies to their process of Resolution.
Certain folks may have experienced the Forewarning and taken subsequent steps to Resolution of most disturbing feelings and may have arrived, after reflection, at a point of peaceful Resolve and accommodation to the reality. They may also have been present at the moment of embarkation by the patient on his or her last and final journey, thus giving them added experience and time to adapt their feelings and responses to what the world around them, incessantly and unrelentingly, requires of everyone regardless of their special human condition at the moment.
From a less forgiving point of view, for others without an inkling of what has been going on around them, there may have been a period of delay, first after the diagnosis and then finding out about the demise after-the-fact, to both of which they might have had Reactions without emotional preparation … and complicated by their own experiences with death. Consider the vast group of people out there who each have their own unique focus on death and what it means to them. There is each individual person's Response to life, to begin with, and then to death, about which they probably don’t give much thought. Given the short amount of time they have been given for Reflection and contemplation about death itself, the death of one's self and the feelings precipitated by the deceased's state of non-existence, they can be caught short on in-depth self-understanding, thoughts about what the family members are going through and the sudden contrasts they are forced to think about in the midst of their busy, self-involved lives.
How does one abruptly stop and shift their focus from their own wants, needs, expectations (of themselves and of others) and instantly, seamlessly begin to have significant thoughts about the wants and needs and behaviors and attitudes of Others while enmeshed and surrounded by soul-shaking concepts like Being and Nothingness? They are at a decided disadvantage, unprepared for the social challenge.
The second focus is the interpersonal interaction between those people who suddenly and unexpectedly are confronted by knowledge of the death and find out from the person who was there at the time of death. These emotionally-charged meetings constitute the situation that precipitated this essay in the first place.
There are two cohorts, i.e., those who just found out after a Short I/D-Time-to-Demise situation and have had no time to process the information, and the other cohort of observers who comprehend the situation, grasp the implications of it and have had time to process and come to terms with those realities.
One cohort has not had an inkling that the situation was this serious (or they have known and been in denial to protect their feelings) (AKA death anxiety or variously referred to as extinction anxiety). Their emotions can spike in a violent startle reaction[5] to the news. The other cohort, usually the medical care-givers, the closest family members and a few other selected persons, have known since the first diagnosis was confirmed by the Treating Medical Team. Besides knowing since the first diagnosis, the Medical Team is less disturbed, having educated the family regarding the seriousness of the situation, and having cared for countless patients in similar terminal situations. The time is long-gone for team members when they were at risk of a startle reaction, fear, psychological breakdown, uncontrollable emotional displays or related behavior. One cohort is not prepared; the other cohort is. Now come the reactions and the interactions [6] about which this essay is concerned.
First a sample reaction: [I note this example based on my belief that “chance favors the prepared mind.” That belief may make this information useful if you get hit with a completely uncontrolled state of affairs] and have to deal with an on-the-spot crisis. For instance, the wild and crazy behavior of a very selfish person whose instant insights may include "their loss," i.e., "their own personal loss ... what They as Survivors Have Lost," almost to the exclusion of the totality of the loss by the deceased patient.” The stage is set for conflict.
Second, a sample of interactions: The family (InGroup) has known, along with the Medical Team, that death was the expected end. But the unknowing survivors, agitated, frightened and emotional, have not known, are not prepared like the InGroup is. They (let’s call them the Not-InGroup) may be aghast at the calm, cool and collected attitude and behavior of the Team, the surviving spouse or other family members. A series of graphic curves may (or may not) help describe the interactions between the InGroup (IG) and the Not-InGroup (NotIG). I have purposely put the graphs and comments at the end so you can just disregard them if they don’t aid understanding. Hint: the curves may represent both/either Understanding Level and/or Anxiety Level and each graph will be described with the appropriate descriptors.
**Different types include, Alzheimer’s, Vascular, Lewy Body, Mixed, Parkinson’s, Frontotemporal Lobe, Creutzfeld-Jakob, Normal pressure hydrocephalus, Huntington’s, Wernicke-Korsakoff Syndrome. 10 Dementia Types Ref Link
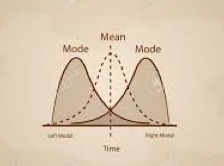
The “Mode” on the left is the InGroup displaying both Reaction to and Reflection on the demise of the patient. The “Mode” on the right represents understanding and / or anxiety of the Not-InGroup.
Focusing on the left InGroup curve and thinking about reactions (to the death), the curve rises quickly to a peak just under the word Mode, then gradually decreases as it drops toward the vertical line labeled “Mean.” The InGroup and Team have marshalled all available resources, applied them to the case and despite their best intentions and advanced applied science, the patient has died. The family et al, being Contemporaneously Supported in every way by the Team, has faced its initial emotions, “worked through them” (whatever that means; different for each individual) and has arrived at a point where they have, in colloquial terms, “been there, done that, don’t need the T-shirt,” and after mourning (or not) have moved on to doing those things which must be done. (In other words, mourning, getting finished with it and carrying on with what life demands of us, sad or happy, in mourning or not. Carrying on with what is normal to life includes behavior after resolution of a traumatic episode, not necessarily “happy” behavior, but expression of that which most folks feel is vastly more important than happiness… that is RELIEF. If you don’t believe Relief is better than happiness, I can’t explain it to you. You had to be there to understand.)
Focusing on the right-side curve, the Not-InGroup curve, the reaction begins to rise before the “Mean” line, but it is still pretty low by the time it crosses the InGroup reaction line.
If we translate the word “reaction” into the word “anxiety,” then we can see that the InGroup anxiety has peaked out and is very low, compared to the Not-InGroup anxiety which is beginning to rise at the intersection of the InGroup line, the Time line and the Not-InGroup line.
So, the In and Not-In groups meet at the intersection… bringing with them all of their Expectations. Like how sad we “should” be, how the family, especially the wife, “should” be dressed in black from head to toe with a black veil so as to avoid displaying her tearful face and blood-shot eyes, and how the children “should” be subdued and the music “should” not be playing the hits of the 70’s (just because they were the favorites of the deceased), and _____________ you fill in the blanks because anything other than the real topic of the day is fair game. And BS-wise, inappropriate.
Because of this intersection (at the memorial service or elsewhere) usually everyone is self-involved with expectations of “what they say” (or don’t say), how they “should” respond (or not) and literally nobody has any framework or psychological construct in mind with which to assess the situation and respond in any personal manner significant to the thoughts and feelings of the survivors. Neither the InGroup nor the Not-InGroup knows what the other is thinking, so the situation is probably a linguistic stand-off governed by lack of mutual knowledge and complicated by their anxiety about “saying the wrong thing.”
It is, therefore, a foregone conclusion that everyone living with “Shoulds” and “Should Nots” rattling around in their heads is going to be part and parcel to some verbal faux-pas or mumbled fumble, some anxiety-driven superficial comment blurted out or a major miscue while trying to avoid talking about “the elephant in the room,” i.e., the deceased, the cruelty of the world’s chronic diseases, why we can’t end everyone’s suffering by legalizing euthanasia and, by the way, have you stocked up like I have with enough excess pills to do myself in so I won’t do to my family what your husband / wife with dementia did to you? No, of course not. But you might consider it, understanding how slowly the social norms of society c h a n g e.
This whole exercise is simply a multi-page way of using verbal and graphic analysis to support giving permission to the members of the family to get the hell away from the intersection of Shoulds and Should Nots. Turn slowly away from the person dumping their expectations or opinions on you, while not uttering even a grunt or comment about why you are leaving the intersection (it’s a free world and you can leave without explanation) and, because you totally understand what is going on at this and other intersections, think to yourself:
“I thank God I am who I am, I can believe and behave how I like, this is MY event, not anyone else’s, and I don’t have to put up with you or anyone else telling me what I should wear or how I should behave. It’s none of your XXX XXXX business, so take a flying leap.”
But don’t waste a word or a breath or a minute of your own precious life on anyone with used oats for brains.
Yeah? Yeah! I got it!
Other situations graphically represented
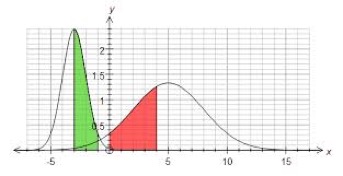
InGroup (green) Not-InGroup (red): IG has strong feelings, but resolves them before the Not-IG tumbles to the fact of the loss and begins late to react (verbally, in print or email) after-the-fact in a public manner without any consideration for the reflection (by the family et al) that has led to the resolution of the distress.
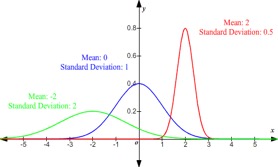
InGroup (green) Not-InGroup (red) Other (blue): alternative intersections with which the InGroup (especially family members) might be confronted (green-blue), (green-red) each of which might lead to interpersonal discussions of very different sorts, depending upon the emotional state of the InGroup member and the intellect, attitude and understanding by personal experience of the Not-IG person … because …
We are all apt to be confronted by various and sundry folks with unanticipated responses, reactions and (usually) little reflection about their effect on a bereaved person … nor any insight whatsoever about whether the bereaved survivor cares even one little bit about the attitudes of Not-IG folks. Coping by awareness.
Solution (partial): The One-Expectation Ploy
One of the observed, genius-level solutions to this inevitable, but rare clash at the intersections, is to create an atmosphere wherein 99% of the attendees are genuinely pleased to express their support of the surviving spouse and family by arriving with only one expectation: we will intermingle as co-workers do, with joy and relief that the agonizing situation has resolved itself, that we are here to support the family by being here one and all, sharing fun and fond memories accumulated over the years, being attentive to the needs of the family in every way we can be and … here comes the key - to the judgmental bitch on the first page …
“Watch me, I am turning away from you, never to return, and in my head and in my heart I am shouting out loud ‘I don’t care about you, except to the level that I am thinking Go Fxxx Yourself and We’re Done Here With The Likes Of You because we know that everyone faced with caring for a person with chronic disease has worked through all the stages, all the feelings, all the regret and remorse, all of the acceptance of the fact that there is nothing else we can do at this point, other than feel the Relief that we deserve, and know that we shun all the Busy-Bs who come to judge and we pray each night that those B-Bs will all go the way of all flesh, leaving us and our room full of joyous supporters to carry on just like our loved one expected of us and like we expect of ourselves.”
[2] https://en.wikipedia.org/wiki/Lingchi ["... Lingchi was used as torture in China 900 CE until it was banned in 1905"]
[3] https://en.wikipedia.org/wiki/Death_by_a_Thousand_Cuts_(book) Which contains a comment about the book by: Jonathan Mirsky in Literary Review (who wrote) that "this is a book primarily about torment."
[4] Link to Hospice Care information
[5] A person, affected by the ailment of exaggerated startle response may have sudden and high startle reactions such as body spasms or eye blinking to unexpected or sudden frightening information, noise, touch or movement. Hypertonia or severe muscle strain or stiffness is observed in the individuals who are affected with exaggerated startle response.
[6] Link to pages on "The Process of Dealing with Death"

- This page was last updated on March 4, 2019.
[The author has had the very painful and prolonged personal experience of watching the slow death of his wife and has shared every one of those "thousand cuts" with her as she physically and mentally deteriorated over a period of many years before her final demise. Thus, you can appreciate the powerful and emotional response to the insensitivity of the woman who is quoted at the beginning of the essay. - Ed.]
Disclaimer | Privacy Policy | Copyright | Sitemap | Contact | Comments










 On this day of giving thanks, I am reminded of all of those who have supported this site over the years. I welcome your comments, your guest articles, and your readership. I am deeply grateful for all…
On this day of giving thanks, I am reminded of all of those who have supported this site over the years. I welcome your comments, your guest articles, and your readership. I am deeply grateful for all…
